News & Events
News
14 February 2024
RTICC Researchers Make Breakthrough in Predicting Immunotherapy Success
The new technology offers a simpler, more precise alternative, allowing physicians to assess a patient's likelihood of benefiting from immunotherapy through a routine blood test
A research team at the Technion's Ruth and Bruce Rappaport Faculty of Medicine has identified blood biomarkers that can predict the effectiveness of immunotherapy in cancer patients. This groundbreaking discovery could significantly improve the process of matching patients to the right immunotherapy treatment, reducing unnecessary side effects for those unlikely to benefit.
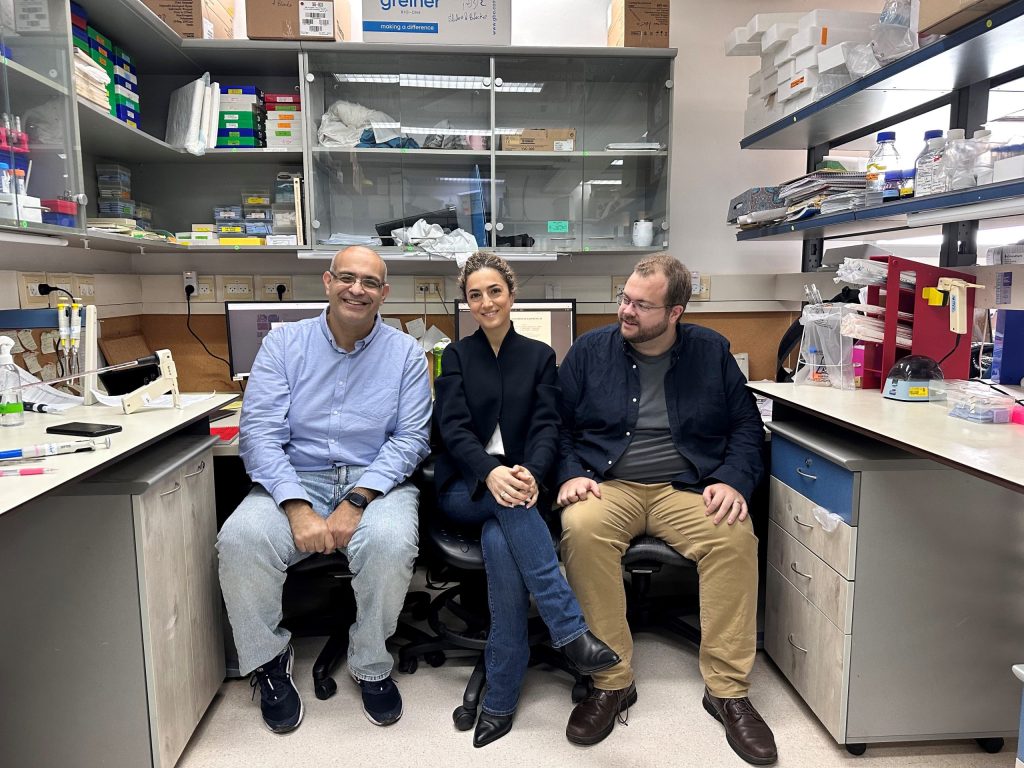
Led by Prof. Yuval Shaked, along with doctoral student Madeleine Benguigui and post-doctoral fellow Dr. Tim J. Cooper, the study focused on RNA sequencing and preclinical cancer models to identify key biomarkers in the bloodstream. These biomarkers, particularly the protein Ly6E(hi) in neutrophils, can predict whether a patient’s immune system will respond effectively to immunotherapy. Unlike traditional biopsy-based methods, this approach relies on blood samples, which are far less invasive and safer for patients.
The researchers found that a protein known as STING, which activates the immune system, is highly present in patients who are likely to respond to immunotherapy. By testing the levels of specific neutrophils in the bloodstream, the team was able to accurately predict patient responses in cases of lung cancer and melanoma. Their findings, which align with data from 1,237 patients, represent a major step forward in personalized cancer treatment.
Current methods of predicting immunotherapy success, like genetic signatures or tumor biopsies, are invasive and often fall short in accuracy. The Technion team's new technology offers a simpler, more precise alternative, allowing physicians to assess a patient's likelihood of benefiting from immunotherapy through a routine blood test. This advancement could revolutionize personalized medicine by reducing the number of patients subjected to ineffective and potentially harmful treatments.
The research was supported by a European Research Council (ERC) grant, the Bruce & Ruth Rappaport Cancer Research Center, Israel Science Foundation, National Institutes of Health (USA), Ariane de Rothschild Foundation (Ariane de Rothschild Women’s Doctoral Program scholarship), and the Rappaport Technion Integrated Cancer Center (RTICC) as part of the Steven & Beverly Rubenstein Charitable Foundation Fellowship Fund for Cancer Research.
The Research has been published in the Journal Cancer Cell.




